Sciatica is a symptom. It consists of leg pain, which might feel
like a bad leg cramp, or it can be excruciating, shooting pain that makes
standing or sitting nearly impossible.
The pain might be worse when you sit, sneeze, or cough. Sciatica
can occur suddenly or it can develop gradually. You might also feel weakness,
numbness, or a burning or tingling ("pins and needles") sensation
down your leg, possibly even in your toes. Less common symptoms might include
the inability to bend your knee or move your foot and toes.
What causes sciatica?
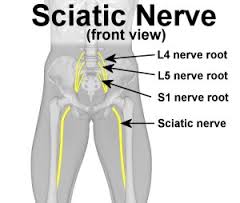
Sciatica might be a symptom of a "pinched nerve"
affecting one or more of the lower spinal nerves. The nerve might be pinched
inside or outside of the spinal canal as it passes into the leg.
Conditions that cause sciatica:
·
A herniated or slipped disc that causes pressure on a nerve root —
This is the most common cause of sciatica.
·
Piriformis syndrome — This develops when the piriformis muscle, a
small muscle that lies deep in the buttocks, becomes tight or spasms, which can
put pressure on and irritate the sciatic nerve.
·
Spinal stenosis — This condition results from narrowing of the
spinal canal with pressure on the nerves.
·
Spondylolisthesis — This is a slippage of one vertebra so that it
is out of line with the one above it, narrowing the opening through which the
nerve exits
How is sciatica diagnosed?
A complete medical history, including a review of your symptoms,
and a physical exam can help the health care provider diagnose sciatica and
determine its cause. For example, he or she might perform a straight-leg-raise
test, in which you lie on your back with your legs straight. The health care
provider will slowly raise each leg and note the elevation at which your pain
begins. This test can help pinpoint the affected nerves and determine if there
is a problem with one of your discs.
Other diagnostic tests might be performed to look for other causes
of sciatic pain. Depending on what your health care provider finds, he or she
might recommend further testing. Such testing might include:
·
X-ray to look for fractures in the spine
·
Magnetic resonance imaging (MRI) or computed tomography (CT) scan
to create images of the structures of the back
·
Nerve conduction velocity studies, evoked potential testing, or
electromyography to examine how well electrical impulses travel through the
sciatic nerve
·
Myelogram using dye injected between the vertebrae to determine if
a vertebra or disc is causing the pain
However, most patients with sciatica can be treated without the
need for further diagnostic testing.
How is sciatica treated?
The goal of treatment is to decrease pain and increase mobility.
Treatment most often includes limited rest (on a firm mattress or on the
floor), physical therapy, and the use of medicine to treat pain and
inflammation. A customized physical therapy exercise program might be
developed.
Medicine — Pain medicines and anti-inflammatory drugs help to relieve
pain and stiffness, allowing for increased mobility and exercise. There are
many common over-the-counter medicines called non-steroidal anti-inflammatory
drugs (NSAIDs). They include aspirin, ibuprofen (Motrin, Advil), and naproxen
(Naprosyn, Aleve).
Muscle relaxants, such as cyclobenzaprine (Flexeril), might be
prescribed to relieve the discomfort associated with muscle spasms. However,
these medicines might cause confusion in older people. Depending on the level
of pain, prescription pain medicines might be used in the initial period of
treatment.
Physical therapy —The goal of physical
therapy is to find exercise movements that decrease sciatic pain by reducing
pressure on the nerve. A program of exercise often includes stretching
exercises to improve flexibility of tight muscles and aerobic exercise, such as
walking.
The therapist might also recommend exercises to strengthen the
muscles of your back, abdomen, and legs.
Spinal injections — An injection of a
cortisone-like anti-inflammatory medicine into the lower back might help reduce
swelling and inflammation of the nerve roots, allowing for increased mobility.
Surgery — Surgery might be needed for people who do not respond to
conservative treatment, who have progressing symptoms, and are experiencing
severe pain.
Surgical options include:
·
Microdiscectomy — This is a procedure
used to remove fragments of a herniated disc.
·
Laminectomy — The bone that curves around and covers the spinal cord
(lamina), and the tissue that is causing pressure on the sciatic nerve are
removed.
Many people believe that yoga or acupuncture can improve sciatica.
Massage might help muscle spasms that often occur along with sciatica.
Biofeedback is an option to help manage pain and relieve stress, which can
affect your ability to cope with pain. These are referred to as alternative
therapies.
What complications are
associated with sciatica?
Chronic (ongoing and lasting) pain is a complication of untreated
sciatica. If the "pinched nerve" is seriously injured, chronic muscle
weakness, such as a "drop foot," might occur.
What is the outlook for
people with sciatica?
Sciatic pain usually goes away with time and rest. Most people
with sciatica (80 percent to 90 percent) will get better without surgery. About
half of affected individuals recover from an episode within six weeks.
Can sciatica be prevented?
Some sources of sciatica are not preventable, such as degenerative
disc disease, back strain due to pregnancy, and accidental falls.
Although it might not be possible to prevent all cases of
sciatica, you can take steps to protect your back and reduce your risk.
·
Practice proper lifting techniques. Lift with your back straight,
bringing yourself up with your hips and legs, and holding the object close to
your chest. Use this technique for lifting everything, no matter how light.
·
Avoid/ stop cigarette smoking, which promotes disc degeneration.
·
Exercise regularly to strengthen the muscles of your back and
abdomen, which work to support your spine.
·
Use good posture when sitting, standing, and sleeping. Good
posture helps to relieve the pressure on your lower back.
·
Avoid sitting for long periods.
© Copyright 1995-2010 The Cleveland Clinic Foundation. All rights
reserved.
1 comment:
Thanks for your lovely post, the contents are quiet interesting. I will be waiting for your next post.
Looking for Pain management in tampa florida
Post a Comment