Breast cancer is a kind of cancer that develops from breast cells. Breast cancer usually starts off in the inner lining of milk ducts or the lobules that supply them with milk. A malignant tumor can spread to other parts of the body. A breast cancer that started off in the lobules is known as lobular carcinoma, while one that developed from the ducts is called ductal carcinoma.
The vast majority of breast cancer cases occur in females. This article focuses on breast cancer in women.
Breast cancer is the most common invasive cancer in females worldwide. It accounts for 16% of all female cancers and 22.9% of invasive cancers in women. 18.2% of all cancer deaths worldwide, including both males and females, are from breast cancer.
Breast cancer rates are much higher in developed nations compared to developing ones. There are several reasons for this, with possibly life-expectancy being one of the key factors - breast cancer is more common in elderly women; women in the richest countries live much longer than those in the poorest nations. The different lifestyles and eating habits of females in rich and poor countries are also contributory factors, experts believe.
The anatomy of a female breast
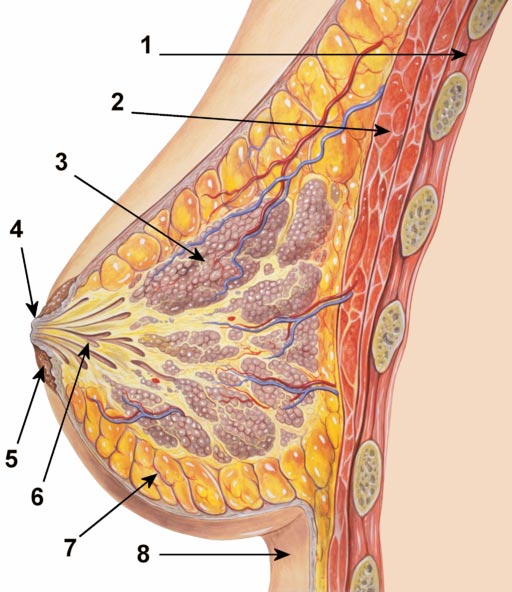
1. Chest wall. 2. Pectoralis muscles. 3. Lobules (glands that make milk). 4. Nipple surface. 5. Areola. 6. Lactiferous duct tube that carries milk to the nipple. 7. Fatty tissue. 8. Skin.
A mature human female's breast consists of fat, connective tissue and thousands of lobules - tiny glands which produce milk. The milk of a breastfeeding mother goes through tiny ducts (tubes) and is delivered through the nipple.
The breast, like any other part of the body, consists of billions of microscopic cells. These cells multiply in an orderly fashion - new cells are made to replace the ones that died. In cancer, the cells multiply uncontrollably, and there are too many cells, progressively more and more than there should be.
Cancer that begins in the lactiferous duct (milk duct), known as ductal carcinoma, is the most common type. Cancer that begins in the lobules, known as lobular carcinoma, is much less common.
What is the difference between invasive and non-invasive breast cancer?
Invasive breast cancer - the cancer cells break out from inside the lobules or ducts and invade nearby tissue. With this type of cancer, the abnormal cells can reach the lymph nodes, and eventually make their way to other organs (metastasis), such as the bones, liver or lungs. The abnormal (cancer) cells can travel through the bloodstream or the lymphatic system to other parts of the body; either early on in the disease, or later.Non-invasive breast cancer - this is when the cancer is still inside its place of origin and has not broken out. Lobular carcinoma in situ is when the cancer is still inside the lobules, while ductal carcinoma in situ is when they are still inside the milk ducts. "In situ" means "in its original place". Sometimes, this type of breast cancer is called "pre-cancerous"; this means that although the abnormal cells have not spread outside their place of origin, they can eventually develop into invasive breast cancer.
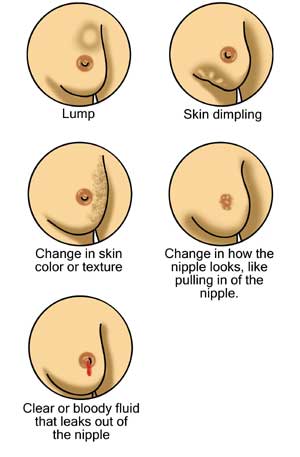
What are the signs and symptoms of breast cancer?
A symptom is only felt by the patient, and is described to the doctor or nurse, such as a headache or pain. A sign is something the patient and others can detect, for example, a rash or swelling.The first symptoms of breast cancer are usually an area of thickened tissue in the woman's breast, or a lump. The majority of lumps are not cancerous; however, women should get them checked by a health care professional.
According to the National Health Service, UK, women who detect any of the following signs or symptoms should tell their doctor:
- A lump in a breast
- A pain in the armpits or breast that does not seem to be related to the woman's menstrual period
- Pitting or redness of the skin of the breast; like the skin of an orange
- A rash around (or on) one of the nipples
- A swelling (lump) in one of the armpits
- An area of thickened tissue in a breast
- One of the nipples has a discharge; sometimes it may contain blood
- The nipple changes in appearance; it may become sunken or inverted
- The size or the shape of the breast changes
- The nipple-skin or breast-skin may have started to peel, scale or flake
What are the causes of breast cancer?
Experts are not sure what causes breast cancer. It is hard to say why one person develops the disease while another does not. We know that some risk factors can impact on a woman's likelihood of developing breast cancer.- Getting older - the older a woman gets, the higher is her risk of developing breast cancer; age is a risk factor. Over 80% of all female breast cancers occur among women aged 50+ years (after the menopause).
- Genetics - women who have a close relative who has/had breast or ovarian cancer are more likely to develop breast cancer. If two close family members develop the disease, it does not necessarily mean they shared the genes that make them more vulnerable, because breast cancer is a relatively common cancer.
The majority of breast cancers are not hereditary.
Women who carry the BRCA1 and BRCA2 genes have a considerably higher risk of developing breast and/or ovarian cancer. These genes can be inherited. TP53, another gene, is also linked to greater breast cancer risk. - A history of breast cancer - women who have had breast cancer, even non-invasive cancer, are more likely to develop the disease again, compared to women who have no history of the disease.
- Having had certain types of breast lumps - women who have had some types of benign (non-cancerous) breast lumps are more likely to develop cancer later on. Examples include atypical ductal hyperplasia or lobular carcinoma in situ.
- Dense breast tissue - women with more dense breast tissue have a greater chance of developing breast cancer.
- Estrogen exposure - women who started having periods earlier or entered menopause later than usual have a higher risk of developing breast cancer. This is because their bodies have been exposed to estrogen for longer. Estrogen exposure begins when periods start, and drops dramatically during the menopause.
- Obesity - post-menopausal obese and overweight women may have a higher risk of developing breast cancer. Experts say that there are higher levels of estrogen in obese menopausal women, which may be the cause of the higher risk.
- Height - taller-than-average women have a slightly greater likelihood of developing breast cancer than shorter-than-average women. Experts are not sure why.
- Alcohol consumption - the more alcohol a woman regularly drinks, the higher her risk of developing breast cancer is.
- Radiation exposure - undergoing X-rays and CT scans may raise a woman's risk of developing breast cancer slightly. Scientists at the Memorial Sloan-Kettering Cancer Center found that women who had been treated with radiation to the chest for a childhood cancer have a higher risk of developing breast cancer. (Link to article)
- HRT (hormone replacement therapy) - both forms, combined and estrogen-only HRTtherapies may increase a woman's risk of developing breast cancer slightly. Combined HRT causes a higher risk.
- Certain jobs - French researchers found that women who worked at night prior to a first pregnancy had a higher risk of eventually developing breast cancer. (Link to article)
Canadian researchers found that certain jobs, especially those that bring the human body into contact with possible carcinogens and endocrine disruptors are linked to a higher risk of developing breast cancer. Examples include bar/gambling, automotive plastics manufacturing, metal-working, food canning and agriculture. They reported their findings in the November 2012 issue of Environmental Health. - Cosmetic implants may undermine breast cancer survival - women who have cosmetic breast implants and develop breast cancer may have a higher risk of dying prematurely form the disease compared to other females, researchers from Canada reported in the BMJ (British Medical Journal) (May 2013 issue).
The team looked at twelve peer-reviewed articles on observational studies which had been carried out in Europe, the USA and Canada.
Experts had long-wondered whether cosmetic breast implants might make it harder to spot malignancy at an early stage, because they produce shadows on mammograms.
In this latest study, the authors found that a woman with a cosmetic breast implant has a 25% higher risk of being diagnosed with breast cancer when the disease has already advanced, compared to those with no implants.
Women with cosmetic breast implants who are diagnosed with breast cancer have a 38% higher risk of death from the disease, compared to other patients diagnosed with the same disease who have no implants, the researchers wrote.
After warning that there were some limitations in the twelve studies they looked at, the authors concluded "Further investigations are warranted into the long term effects of cosmetic breast implants on the detection and prognosis of breast cancer, adjusting for potential confounders."
Diagnosing breast cancer
Women are usually diagnosed with breast cancer after a routine breast cancer screening, or after detecting certain signs and symptoms and seeing their doctor about them.If a woman detects any of the breast cancer signs and symptoms described above, she should speak to her doctor immediately. The doctor, often a primary care physician (general practitioner, GP) initially, will carry out a physical exam, and then refer the patient to a specialist if he/she thinks further assessment is needed.
Below are examples of diagnostic tests and procedures for breast cancer:
- Breast exam - the physician will check both the patient's breasts, looking out for lumps and other possible abnormalities, such as inverted nipples, nipple discharge, or change in breast shape. The patient will be asked to sit/stand with her arms in different positions, such as above her head and by her sides.
- X-ray (mammogram) - commonly used for breast cancer screening. If anything unusual is found, the doctor may order a diagnostic mammogram.
Breast cancer screening has become a controversial subject over the last few years. Experts, professional bodies, and patient groups cannot currently agree on when mammography screening should start and how often it should occur. Some say routine screening should start when the woman is 40 years old, others insist on 50 as the best age, and a few believe that only high-risk groups should have routine screening.
In July, 2012, The American Medical Association said that women should be eligible for screening mammography from the age of 40, and it should be covered by insurance.
In a Special Report in The Lancet (October 30th, 2012 issue), a panel of experts explained that breast cancer screening does reduce the risk of death from the disease. However, they added that it also creates more cases of false-positive results, where women end up having unnecessary biopsies and harmless tumors are surgically removed.
Another study, carried out by scientists at the The Dartmouth Institute for Healthy Policy & Clinical Practice in Lebanon, N.H., and reported in the New England Journal of Medicine(November 2012 issue), found that mammograms do not reduce breast cancer death rates.
A team from the University of Copenhagen reported that women who have false-positive mammogram outcomes may suffer long-lasting stress and anxiety, in some cases this can last up to three years. They published their findings in Annals of Family Medicine (March 2013 issue).
Researchers from the Barbara Ann Karmanos Cancer Institute in Detroit, Michigan, found that breast cancer mortality was higher among older women whose time-lapses between their last mammogram and their breast cancer diagnosis were longer. They presented their findings at the American Association for Cancer Research (AACR) Annual Meeting 2013.
Team leader, Michael S. Simon, M.D., M.P.H., said "We found that for women age 75 and older, a longer time interval between the last mammogram and the date of breast cancer diagnosis was associated with a greater chance for dying from breast cancer." - 2D combined with 3D mammograms - 3D mammograms, when used in collaboration with regular 2D mammograms were found to reduce the incidence of false positives, researchers from the University of Sydney's School of Public Health, Australia, reported inThe Lancet Oncology.
The researchers screened 7,292 adult females, average age 58 years. Their initial screening was done using 2D mammograms, and then they underwent a combination of 2D and 3D mammograms.
Professor Nehmat Houssami and team found 59 cancers in 57 patients. 66% of the cancers were detected in both 2D and combined 2D/3D screenings. However, 33% of them were only detected using the 2D plus 3D combination.
The team also found that 2D plus 3D combination screenings were linked to a much lower number of false positives. When using just 2D screenings there were 141 false positives, compared to 73 using the 2D plus 3D combination.
Prof. Houssami said "Although controversial, mammography screening is the only population-level early detection strategy that has been shown to reduce breast cancer mortality in randomized trials. Irrespective of which side of the mammography screening debate one supports, efforts should be made to investigate methods that enhance the quality of, and hence potential benefit from, mammography screening.
We have shown that integrated 2D and 3D mammography in population breast-cancer screening increases detection of breast cancer and can reduce false-positive recalls depending on the recall strategy. Our results do not warrant an immediate change to breast-screening practice, instead, they show the urgent need for randomised controlled trials of integrated 2D and 3D versus 2D mammography." - Beast ultrasound - this type of scan may help doctors decide whether a lump or abnormality is a solid mass or a fluid-filled cyst.
- Biopsy - a sample of tissue from an apparent abnormality, such as a lump, is surgically removed and sent to the lab for analysis. It the cells are found to be cancerous, the lab will also determine what type of breast cancer it is, and the grade of cancer (aggressiveness). Scientists from the Technical University of Munich found that for an accurate diagnosis, multiple tumor sites need to be taken. (Link to article)
- Breast MRI (magnetic resonance imaging) scan - a dye is injected into the patient. This type of scan helps the doctor determine the extent of the cancer. Researchers from the University of California in San Francisco found that MRI provides a useful indication of a breast tumor's response to pre-surgical chemotherapy much earlier than possible through clinical examination. (Link to article)
A cancer's stage is a crucial factor in deciding what treatment options to recommend, and in determining the patient's prognosis.
Staging is done after cancer is diagnosed. To do the staging, the doctor may order several different tests, including blood tests, a mammogram, a chest X-ray, a bone scan, a CT scan, or a PET scan.
What are the treatment options for breast cancer?
A multidisciplinary team will be involved in a breast cancer patient's treatment. The team may consists of an oncologist, radiologist, specialist cancer surgeon, specialist nurse, pathologist, radiologist, radiographer, and reconstructive surgeon. Sometimes the team may also include an occupational therapist, psychologist, dietitian, and physical therapist.The team will take into account several factors when deciding on the best treatment for the patient, including:
- The type of breast cancer
- The stage and grade of the breast cancer - how large the tumor is, whether or not it has spread, and if so how far
- Whether or not the cancer cells are sensitive to hormones
- The patient's overall health
- The age of the patient (has she been through the menopause?)
- The patient's own preferences
- Radiation therapy (radiotherapy)
- Surgery
- Biological therapy (targeted drug therapy)
- Hormone therapy
- Chemotherapy
- Lumpectomy - surgically removing the tumor and a small margin of healthy tissue around it. In breast cancer, this is often called breast-sparing surgery. This type of surgery may be recommended if the tumor is small and the surgeon believes it will be easy to separate from the tissue around it. British researchers reported that about one fifth of breast cancer patients who choose breast-conserving surgery instead of mastectomy eventually need a reoperation. (Link to article)
- Mastectomy - surgically removing the breast. Simple mastectomy involves removing the lobules, ducts, fatty tissue, nipple, areola, and some skin. Radical mastectomy means also removing muscle of the chest wall and the lymph nodes in the armpit.
- Sentinel node biopsy - one lymph node is surgically removed. If the breast cancer has reached a lymph node it can spread further through the lymphatic system into other parts of the body.
- Axillary lymph node dissection - if the sentinel node was found to have cancer cells, the surgeon may recommend removing several nymph nodes in the armpit.
- Breast reconstruction surgery - a series of surgical procedures aimed at recreating a breast so that it looks as much as possible like the other breast. This procedure may be carried out at the same time as a mastectomy. The surgeon may use a breast implant, or tissue from another part of the patient's body.
Controlled doses of radiation are targeted at the tumor to destroy the cancer cells. Usually, radiotherapy is used after surgery, as well as chemotherapy to kill off any cancer cells that may still be around. Typically, radiation therapy occurs about one month after surgery or chemotherapy. Each session lasts a few minutes; the patient may require three to five sessions per week for three to six weeks.
The type of breast cancer the woman has will decide what type of radiation therapy she may have to undergo. In some cases, radiotherapy is not needed.
Radiation therapy types include:
- Breast radiation therapy - after a lumpectomy, radiation is administered to the remaining breast tissue
- Chest wall radiation therapy - this is applied after a mastectomy
- Breast boost - a high-dose of radiation therapy is applied to where the tumor was surgically removed. The appearance of the breast may be altered, especially if the patient's breasts are large.
- Lymph nodes radiation therapy - the radiation is aimed at the axilla (armpit) and surrounding area to destroy cancer cells that have reached the lymph nodes
- Breast brachytherapy - scientists at UC San Diego Moores Cancer Center revealed that patients with early-stage breast cancer in the milk ducts which has not spread, seem to benefit from undergoing breast brachytherapy with a strut-based applicator. This 5-day treatment is given to patients after they have undergone lumpectomy surgery. The researchers found that women who received strut-based breast brachytherapy had lower recurrence rates, as well as fewer and less severe side effects. (Link to article)
Chemotherapy
Medications are used to kill the cancer cells - these are called cytotoxic drugs. The oncologist may recommend chemotherapy if there is a high risk of cancer recurrence, or the cancer spreading elsewhere in the body. This is called adjuvant chemotherapy.
If the tumors are large, chemotherapy may be administered before surgery. The aim is to shrink the tumor, making its removal easier. This is called neo-adjuvant chemotherapy.
Chemotherapy may also be administered if the cancer has metastasized - spread to other parts of the body. Chemotherapy is also useful in reducing some of the symptoms caused by cancer.
Chemotherapy may help stop estrogen production. Estrogen can encourage the growth of some breast cancers.
Side effects of chemotherapy may include nausea, vomiting, loss of appetite, fatigue, sore mouth, hair loss, and a slightly higher susceptibility to infections. Many of these side effects can be controlled with medications the doctor can prescribe. Women over 40 may enter early menopause.
Protecting female fertility - Scientists have designed a way of aggressively attacking cancer with an arsenic-based chemo medication, which is much gentler on the ovaries. The researchers, from Northwestern University Feinberg School of Medicine in Chicago, believe their novel method will help protect the fertility of female patients undergoing cancer treatment.
The scientists say they also developed a way of rapidly testing existing chemotherapy drugs for their effect on ovarian function, so that doctors and patients can make decisions regarding treatment that minimize damage to ovaries.
They reported their findings in the journal PLOS ONE (March 2013 issue). The authors claim that the new nanoparticle chemo medication they designed is the first cancer drug to be tested during development for its impact on fertility using the new rapid toxicity test.
Although more cancer patients are surviving today thanks to the advances in cancer therapies, a significant number of female patients still face fertility loss after undergoing traditional chemotherapy.
Co-principal study investigator Teresa Woodruff, said "Our overall goal is to create smart drugs that kill the cancer but don't cause sterility in young women."
Hormone therapy (hormone blocking therapy)
Used for breast cancers that are sensitive to hormones. These types of cancer are often referred to as ER positive (estrogen receptor positive) and PR positive (progesterone receptor positive) cancers. The aim is to prevent cancer recurrence. Hormone blocking therapy is usually used after surgery, but may sometimes be used beforehand to shrink the tumor.
If for health reasons, the patient cannot undergo surgery, chemotherapy or radiotherapy, hormone therapy may be the only treatment she receives.
Hormone therapy will have no effect on cancers that are not sensitive to hormones.
Hormone therapy usually lasts up to five years after surgery.
The following hormone therapy medications may be used:
- Tamoxifen - prevents estrogen from binding to ER-positive cancer cells. Side effects may include changes in periods, hot flashes, weight gain, headaches, nausea, vomiting, fatigue, and aching joints.
A biomarker in breast cancer patients who do not respond, or who have become resistant to Tamoxifen has been discovered by researchers at the University of Manchester, England. They say that their discovery will help doctors decide which patients are suitable or not for adjuvant (complementary) hormone therapy with Tamoxifen. - Aromatase inhibitors - this type of medication may be offered to women who have been through the menopause. It blocks aromatase. Aromatase helps estrogen production after the menopause. Before the menopause, a woman's ovaries produce estrogen. Examples of aromatase inhibitors include letrozole, exemestane, and anastrozole. Side effects may include nausea, vomiting, fatigue, skin rashes, headaches, bone pain, aching joints, loss of libido, sweats, and hot flashes.
Ovarian ablation or suppression - pre-menopausal women produce estrogen in their ovaries. Ovarian ablation or suppression stop the ovaries from producing estrogen. Ablation is done either through surgery or radiation therapy - the woman's ovaries will never work again, and she will enter the menopause early.
A luteinising hormone-releasing hormone agonist (LHRHa) drug called Goserelin will suppress the ovaries. The patient's periods will stop during treatment, but will start again when she stops taking Goserelin. Women of menopausal age (about 50 years) will probably never start having periods again. Side effects may include mood changes, sleeping problems, sweats, and hot flashes.
- Trastuzumab (Herceptin) - this monoclonal antibody targets and destroys cancer cells that are HER2-positive. Some breast cancer cells produce large amounts of HER2 (growth factor receptor 2); Herceptin targets this protein. Possible side effects may include skin rashes, headaches, and/or heart damage.
- Lapatinib (Tykerb) - this drug targets the HER2 protein. It is also used for the treatment of advanced metastatic breast cancer. Tykerb is used on patients who did not respond well to Herceptin. Side effects include painful hands, painful feet, skin rashes, mouth sores, extreme tiredness, diarrhea, vomiting, and nausea.
- Bevacizumab (Avastin) - stops the cancer cells from attracting new blood vessels, effectively causing the tumor to be starved of nutrients and oxygen. Side effects may include congestive heart failure, hypertension (high blood pressure), kidney damage, heart damage, blood clots, headaches, mouth sores. Although not approved by the FDA for this use, doctors may prescribe it "off-label". Using this drug for breast cancer is controversial. The FDA in 2011 said that Avastin is neither effective nor safe for breast cancer. (Link to article)
Swiss researchers found that Avastin offers only a modest benefit regarding disease progression in women with advanced stage breast cancer. They added that it has no impact on survival. (Link to article) - Low dose aspirin
Research carried out on laboratory mice and test tubes suggests that regular low-dose aspirin may halt the growth and spread of breast cancer.
Scientists from the Veterans Affairs Medical Center in Kansas City and the University of Kansas Medical Center explained that their tests on cancer lines and in mice showed thataspirin not only slowed the growth of cancer cells and shrank tumors considerably, but also stopped metastasis (cancer spreading to new sites).
Their research involved assessing aspirin's effects on two types of cancer, including the aggressive "triple-negative" breast cancer which is resistant to most current treatments.
Cancer campaigners cautioned that although the current results show great promise, this research is at a very early stage and has yet to be shown to be effective on humans.
Preventing breast cancer
Some lifestyle changes can help significantly reduce a woman's risk of developing breast cancer.- Alcohol consumption - women who drink in moderation, or do not drink alcohol at all, are less likely to develop breast cancer compared to those who drink large amounts regularly. Moderation means no more than one alcoholic drink per day.
- Physical exercise - exercising five days a week has been shown to reduce a woman's risk of developing breast cancer. Researchers from the University of North Carolina Gillings School of Global Public Health in Chapel Hill reported that physical activity - either mild or intense and before or after menopause - can lower breast cancer risk, but considerable weight gain may negate these benefits. (Link to article)
- Diet - some experts say that women who follow a healthy, well-balanced diet may reduce their risk of developing breast cancer.
- Postmenopausal hormone therapy - limiting hormone therapy may help reduce the risk of developing breast cancer. It is important for the patient to discuss the pros and cons thoroughly with her doctor.
- Bodyweight - women who have a healthy bodyweight have a considerably lower chance of developing breast cancer compared to obese and overweight females.
- Women at high risk of breast cancer - the doctor may recommend estrogen-blocking drugs, including tamoxifen and raloxifene. Tamoxifen may raise the risk of uterine cancer. Preventive surgery is a possible option for women at very high risk.
- Breast cancer screening - patients should discuss with their doctor when to start breast cancer screening exams and tests.
- Breastfeeding - women who breastfeed run a lower risk of developing breast cancer compared to other women.
Survivors of breast cancer and diabetes risk
Postmenopausal women who survived breast cancer are more likely to develop diabetes, compared to other women of their age who did not have breast cancer, researchers from the Women's College Hospital, Women's College Research Institute, Toronto, reported in the journal Diabetologia.The authors added that breast cancer survivors who had undergone chemotherapy were especially at risk of developing diabetes.
Over the last few years, scientists have become increasingly aware of a link between cancer and diabetes. The association works the other way round too - women with diabetes are 20% more likely to develop breast cancer after the menopause compared to their counterparts who are not diabetic.
More women are surviving breast cancer, experts say, making it much more important to understand what the long-term outcomes for survivors are as they grow older.
Written by Christian Nordqvist
Original article date: 5 February 2006. Article updated: 14th December 2012
Copyright: Medical News Today